London, England and Boston, MA – June 7, 2024 – Calyx / Invicro, a global leader in providing medical imaging solutions and development services to the clinical research community, today announces a strategic partnership with BAMF Health, a world leader in molecular imaging and theranostics. The partnership aims to accelerate the clinical translation of radioligand therapies (RLT) and immuno-oncology (IO) agents.
This collaboration addresses challenges caused by fragmented service ecosystems, which have led to duplicative efforts, slow knowledge transfer, and prolonged development timelines. By combining Calyx / Invicro’s radiochemistry and imaging biomarker solutions with BAMF Health’s advanced radiopharmacy facility—which supports a range of alpha, beta, and gamma agents, and molecular imaging and therapy clinics—biotech and pharmaceutical companies now have an end-to-end resource for translating these advanced programs into clinical trials.
A catalyzing project for this partnership is an actinium-225 initiative, for which TerraPower is supplying actinium-225, and BAMF is leveraging its GE HealthCare StarGuide™ SPECT/CT and dosimetry expertise to enhance the study and application of actinium-225 in RLT.
This association represents a key moment in our industry, as contract research organizations, contract manufacturing organizations, and imaging clinics must collaborate more than ever to support these complicated and technically demanding RLT and IO programs. This collaboration and working relationship streamlines operations with easier contracting and communication, brings together knowledge across scientific, regulatory, and operational areas, and provides access to the latest technologies from early preclinical research to patient imaging.
“The success of Calyx / Invicro’s translational model in the CNS field, demonstrated at our London and New Haven clinics, shows the effectiveness of an integrated service approach. We believe our partnership with BAMF Health will bring the same level of innovation and acceleration to oncology,” said Edward Hogan, COO of Calyx / Invicro.
BAMF Health’s Director of Clinical Trials, Dan Rogers, added, “Combining our strengths with Calyx / Invicro allows us to tackle the unique challenges of developing radioligand and immuno-oncology therapies. This collaboration is set to enhance and speed up the development process, towards our mission of making precision medicine available and affordable to everyone.”
Through this partnership, Calyx / Invicro and BAMF Health aim to tackle key hurdles in the clinical translation of radioligand and immuno-oncology treatments. Their combined efforts highlight a commitment to advancing these therapies, redefining oncology care standards, and ensuring faster access to promising treatments for patients.
For more information on Calyx’s experience in oncology trial imaging, visit Oncology Imaging Services| Calyx.
About Calyx / Invicro
Calyx / Invicro is a trusted global provider of scientific and medical expertise for imaging strategy, implementation, and analysis in clinical trials. The organizations have combined to create a new global leader in the provision of medical imaging solutions and to deliver the broadest range of preclinical – late-phase imaging services in the industry, including imaging biomarkers, core lab services, analytics, and software.
With operations in six countries, Calyx / Invicro helps global pharmaceutical, biotech, and contract research organizations achieve their development objectives in key therapeutic areas including oncology, central nervous system, and respiratory, and is meeting the growing demand for enhanced imaging and new therapies in fast-growing specialties such as radiotherapy, gastroenterology, inflammation, fibrosis, and mitochondrial imaging.
Visit Calyx.ai and Invicro.com for more information.
About BAMF Health
BAMF Health is the world’s first vertically integrated platform for intelligence-based precision medicine. Headquartered in Grand Rapids, Michigan, BAMF Health employs the most advanced theranostic imaging technology to detect and treat cancer and other diseases and conduct advanced clinical trials. Our overriding mission is to empower patients to become people again. With a team of data scientists, researchers, software engineers, and clinicians — all working in lockstep— we’re making good on it. To learn more about BAMF Health, visit www.bamfhealth.com.
media contacts:
Morgan Horner | Product Marketing Manager, Invicro | Mhorner@invicro.com
Christine Van Timmeren | Marketing and Communications Manager, BAMF Health | Christine.vantimmeren@bamfhealth.com
The current lack of objective biomarkers presents a real challenge for researchers developing treatments for psychiatric and neurological diseases. But now, a partnership that combines Calyx’s clinical trial imaging expertise and Ceretype’s novel functional MRI (fMRI) platform enables trial sponsors to overcome this challenge and see the objective outcome of a drug on patients with psychiatric and other neurological disorders.
Here we talk with Ceretype CEO and co-founder, Emily Stern about how fMRI can improve CNS clinical trials and how the partnership with Calyx Medical Imaging is greater than the sum of its parts.
What does Ceretype do?
Ceretype is focused on translating fMRI scanning into clinically useful products. For a long time, fMRI has been a powerful tool for research in academic medicine, enabling investigators to learn more about normal brain function and dysfunction in disease settings. However, the methodology hasn’t translated out of academia for several reasons, which Ceretype has now addressed.
An important part of Ceretype’s roadmap is to use fMRI technology to improve the outcomes of CNS clinical trials, an area in which we can immediately supply critical biological insights about the brain and how treatments impact its function.
What is the difference between fMRI and traditional MRI?
fMRI allows us to look at function in addition to structure. It’s a non-invasive tool that measures activity across the entire brain. It’s based on the fact that when nerve cells are active in specific areas of the brain there’s a local increase in blood flow and related changes in blood oxygenation. These result in biochemical changes that fMRI can measure.
With fMRI, we can measure changes in activity that occur while the brain is actively performing a task or at rest . For example, we can see the areas responsible for deciding to move a hand. We can see the areas responsible for speech, hearing/interpreting language, or problem-solving. We can even see the areas that underly emotions. And we can measure and localize abnormal activity associated with brain disease in psychiatry and neurology, or in response to treatment.
Additional Resources
Learn how Calyx and Ceretype are helping researchers understand the mechanisms in the brain that are associated with addictive behavior.
How can fMRI help clinical research and patients?
fMRI has already been a powerful tool in academia, helping us understand the neurobiology that underlies psychiatric and neurologic disorders. But it hasn’t scaled due to several technical hurdles. Ceretype has addressed these challenges systematically to create a scalable, easily deployable, reliable, reproducible, and compliant platform, enabling us to deploy fMRI widely in multi-site clinical trials.
Until now, psychiatry hasn’t had any biological measures to inform drug development or help with patient care, unlike virtually every other area of medicine. So, bringing this technology to psychiatric and other CNS-related clinical trials will be helpful in several ways.
For example, we can objectively measure the impact of an intervention on specific brain networks, allowing us to identify the therapeutic mechanism of action. We can subtype and stratify patients based on criteria such as whether they’ve responded to treatment or not.
We can also de-risk and accelerate trials by identifying more homogeneous patient groups based on brain activity patterns. For example, an important factor in the high failure rate of depression or schizophrenia trials is the heterogeneous biology that makes it unlikely that a drug will work in every patient. Hence, being able to enrich or to stratify the patient samples based on their brain activity patterns can increase the likelihood that the trial will reach significance and potentially get there more quickly. This could be very powerful in psychiatric drug development which, until now, has relied solely on subjective endpoints.
Is there evidence to prove fMRI is beneficial to clinical trials?
Our team has published numerous papers showing our methodology, which includes a technique called multi echo fMRI, significantly increases the signal to noise ratio by a factor of up to four times. The result is substantially more accurate, reliable, and reproducible fMRI. This is a prerequisite for multi-site clinical trials.
We’ve also shown that fMRI can inform our understanding of the neurobiology of multiple neuropsychiatric diseases, such as depression, schizophrenia and post-traumatic stress disorder. We and others have demonstrated that fMRI can show how the brain is modulated in response to different therapies. So, there is a lot of evidence to indicate that this technology will bring value to trials. And having this biological evidence of drug effects, particularly in psychiatry, will be a huge step forward and something that we’re very excited about.
What is the benefit of Calyx’s partnership with Ceretype?
Ceretype and Calyx are truly very complementary. While Ceretype brings this powerful new technology to inform, de-risk, and accelerate clinical trials, Calyx has a mature infrastructure for implementing the technology seamlessly into trial workflows. And Calyx is prescient in seeing the value of bringing these types of technologies to clinical trials. I think that together we’re more than the sum of our parts and we’ll accomplish great things together.
London, England and Boston, MA – May 6 2024 – Calyx, a leading technology-enabled provider of Medical Imaging services and IRT/RTSM (Interactive Response Technology/Randomized Trial Supply Management) today announced its role in supporting the imaging-based endpoint for the pivotal trial that supported the FDA’s groundbreaking approval of Iovance Biotherapeutic’s AMTAGVI™ (lifileucel). Indicated for the treatment of adult patients with unresectable or metastatic melanoma who have relapsed on other front-line therapy, AMTAGVI is the first cell therapy approved to treat solid tumors, which account for 90% of all cancers.
Calyx Medical Imaging contributed to the design and implementation of the imaging components of the accelerated Phase II clinical trial, enabling 60 investigative sites to capture patient images via CT, MRI, PET, and skin photography in compliance with the protocol. Because image review in cell therapy requires thoughtful and strategic scientific implementation, Calyx’s oncology imaging experts designed an image review methodology that enabled uniform and consistent evaluation by Calyx’s independent readers.
“The work that Iovance is doing is extremely important, not only to melanoma patients and their loved ones but also to the broader oncology research community,” said David Herron, CEO of Calyx Medical Imaging. “We are honored to have played a role in this important development program and look forward to continuing our collaboration with the Iovance team.”

David Herron
CEO, Calyx
For more information on Calyx’s experience in oncology trial imaging, visit Oncology Imaging Services| Calyx.
About Calyx
Calyx is a leading global technology-enabled service provider for Medical Imaging and IRT/RTSM (Interactive Response Technology/Randomized Trial Supply Management) for drug developers and the global clinical research community. Calyx’s market-leading service, scientific knowledge, expertise, and technology offering help speed up the delivery of life-saving treatments to millions of patients around the world by accelerating and improving clinical trial outcomes.
With operations in six countries, the company provides 24/7 services to most of the world’s leading pharma and biotech companies.
For more information go to Calyx.ai and follow us on LinkedIn, Twitter, and Facebook.
contact:
Christine Tobin | Calyx | Christine.Tobin@Calyx.ai | +1 412-628-8598
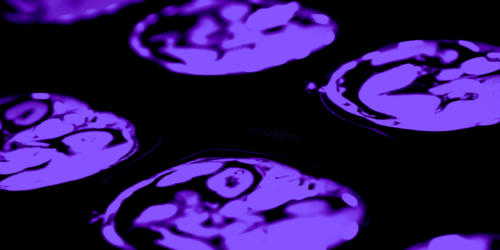
In September 2023, the Journal of Clinical Oncology published, the long-awaited, “RANO 2.0: Update to the Response Assessment in Neuro-Oncology Criteria for High- and Low-Grade Gliomas in Adults.” Intended to overcome the limitations of Response Assessment in Neuro-Oncology (RANO) criteria for high-grade gliomas (RANO-HGG) and low-grade gliomas (RANO-LGG), these revised criteria also address challenges that have emerged when integrating features of the modified RANO (mRANO) or the immunotherapy RANO (iRANO) criteria in imaging assessments in clinical trials.
Here we review key considerations for utilizing RANO criteria in assessing glioblastoma treatments.
Image Acquisition
Contrast-enhanced brain MRI should be acquired per Brain Tumor Imaging Protocol (BTIP) (Ellingson et al, Neuro-Oncology, 2015). Pre- and post-contrast T1w imaging (slice thickness ≤ 1.5 mm) and T2w / FLAIR (slice thickness ≤ 4 mm) in axial plane are required; supplementary planes are highly recommended. Ideally, scanner, sequence, and acquisition parameter consistency are recommended for the accuracy of longitudinal assessments.
Going to ASCO 2024?
Meet Calyx’s Medical Imaging Experts at Booth 10098
Additional Resources
Learn how Calyx de-risks glioblastoma trial imaging

“The introduction of RANO 2.0 will drive consistency for researchers and regulators in the evaluation of product efficacy.”
– Elif Sikoglu, PhD, Sr. Medical Director, Calyx
Choosing the Assessment Criteria
The presentation of disease at baseline and over time can vary significantly depending on the type of brain tumor. Despite glioblastomas being solitary tumors, they often have different morphologies and may contain multiple regions in different stages of malignant degeneration. Hence, it is critical to select and diligently implement the right criteria for disease assessment in glioblastoma clinical trials (i.e. RANO-HGG vs. RANO-LGG vs. modified RANO (mRANO) vs. immunotherapy RANO (iRANO)).
RANO 2.0 criteria authors intend to unite all the earlier RANO versions into one, for all grades of IDH-mutated gliomas, and other glial tumors, regardless of the specific therapies being evaluated. However, this unification still holds some additional considerations due to the complexities of brain tumors and their potential treatments.
For example, for HGG the enhancing disease as captured in contrast-enhanced T1w imaging would represent the disease, and bi-dimensional measurement on the most representative slice would be sufficient to capture the cross-sectional area, i.e., the state of the disease and its change over time. For LGG, the entirety of the tumor (i.e. including non-enhancing) as captured in T2w/FLAIR may be needed and due to the characteristics of the typical LGG over time, volumetric characterization at each time point may still be needed
Highlights from RANO 2.0
- Use post-radiotherapy scan as baseline:Especially for newly diagnosed glioblastoma, the post-radiotherapy MRI (~4 weeks post from the end of radiotherapy) as opposed to post-surgery MRI, will be utilized as baseline to evaluate the disease progression and/or treatment response. This approach assumes that clinical trial randomization will take place after radiotherapy. For patients not undergoing radiotherapy, the post-surgery MRI will be used as the baseline. The duration between the baseline scans and the initiation of therapy should not exceed 2 weeks.
- Confirmation of PD scan 3 months post-radiotherapy: Additional confirmatory scans (at 4- or 8-week intervals) are required for treatment decisions due to high incidence of pseudoprogression within 12 weeks after radiotherapy. In addition, for treatments with a high likelihood of pseudoprogression, mandatory confirmation of progression with a repeat MRI is highly recommended to prevent pre-mature progression determination.
- Two-dimensional measurements remain the accepted approach for quantification of disease cross-sectional area for capturing the enhancing lesions for HGG as well as non-contrast enhancing lesions for LGG. The more advanced approaches, including volumetric assessments, diffusion and/or perfusion imaging or PET imaging, remain valuable options to provide further insight. However, these additional assessments come with challenges regarding the implementation of acquisition and assessments within multi-site clinical trials, resulting in additional cost and study complexity.
- Clinical deterioration as well as corticosteroid information remain crucial components for response assessment. Further guidance on the adaptation of the Neurologic Assessment in Neuor-Oncology (NANO) scale can benefit further standardization of assessments.
Conclusion
The introduction of RANO 2.0 is a positive step for glioblastoma assessments within clinical trials as it will drive consistency for researchers and regulators in the evaluation of product efficacy. However, for optimum efficacy assessment, it remains critical for researchers to consider the specifics of the patient population, study design, as well as the treatment approach, and to adapt the needed nuances in the application of criteria.
Calyx, a leading technology-enabled provider of Medical Imaging services and IRT/RTSM (Interactive Response Technology/Randomized Trial Supply Management) to drug developers, and Invicro, a next-generation quantitative imaging biomarker company and pre-eminent development partner to pharma sponsors, have agreed to combine their businesses. This complementary combination will create a new global leader in the provision of medical imaging solutions and development services to the clinical research community.
The enlarged Group (“Group”) formed through this strategic combination will see 100% of Invicro being acquired by Calyx from its current owner, REALM IDx, Inc. The transaction is subject to regulatory filings and customary closing conditions and is expected to complete in Q2 2024.
Calyx and Invicro each provide complementary services to most of the world’s leading pharma and biotechnology companies. The Group will employ approximately 2,000 highly skilled employees across ten sites, throughout the US, Europe and Asia, thereby having the ability to provide a full suite of solutions to its clients across the world. The combination unites deep heritage and extensive experience reflected in combined support for almost 12,000 clinical and research trials to date, across all clinical phases, including oncology and the central nervous system (CNS). The Group will also boast deep research and development capabilities to provide scientific and service support in the preclinical and exploratory work of its clients.
Commenting on the transaction, David Herron, CEO of Calyx, said: “Calyx and Invicro are uniquely complementary businesses in terms of their scientific talent, service offerings, and international presence. This exciting union will create a truly differentiated industry leader and provides a clear response to growing customer requirements for broader support. Our leadership will be evident in terms of the Group’s global reach across the US, Europe and Asia, and, critically, our extensive scientific knowledge, capabilities and experience. This combined expertise and broader best-in-class specialist support creates a compelling customer proposition for the greater biopharma industry, ranging from large pharma companies to specialty biotech firms. This spans the complete R&D lifecycle from discovery through research and development to post-marketing, across a number of areas including imaging biomarkers, core lab services, analytics and software.”

David Herron
CEO, Calyx
Edward Hogan, COO of Invicro, said: “We are very excited about the impending combination of our two companies. We see huge opportunity in uniting highly skilled teams of scientists and researchers to enable us to work more closely with our partners. Our work will help accelerate the development of new life-saving therapies to provide better outcomes for patients. We can do this across key therapeutic areas, including oncology and the central nervous system (CNS), including unique specialist radioligand therapy capabilities to meet the growing demand for enhanced imaging and new treatments in fast-growing specialties such as radiotherapy, gastroenterology, inflammation, fibrosis and mitochondrial imaging.”
Post completion of the transaction, the process to combine and integrate the two companies will commence. During this period the focus will be on ensuring that customers receive the same high-quality service and support that they have been accustomed to receiving from both Calyx and Invicro.
For more information please contact:
Paul Griffin | Reputation Inc | pgriffin@reputation-inc.com | +353 87 667 4305
Christine Tobin | Calyx | Christine.Tobin@Calyx.ai | +1 412-628-8598
About Calyx
Calyx is a leading global technology-enabled service provider for medical imaging and IRT/RTSM (Interactive Response Technology/Randomised Trial Supply Management) for drug developers and the global clinical research community. Calyx’s market-leading service, scientific knowledge, expertise and technology offering helps speed up the delivery of life-saving treatments to millions of patients around the world by accelerating and improving clinical trial outcomes. With operations in six countries, the company provides 24/7 services to most of the world’s leading pharma and biotech companies.
About Invicro
Headquartered in the US, Invicro is a next-generation quantitative imaging biomarker company focused on accelerating the discovery and development of life-changing medicines. With laboratories in the US, UK, India, Japan and China, Invicro is global research partner to numerous pharmaceutical, biotech and contract research organizations, leveraging its platform to combine best-in-class expertise, imaging biomarkers, core lab services, analytics, and software. Its medical imaging capabilities are helping to achieve better patient outcomes in key therapeutic areas including oncology, central nervous system and respiratory, as well as meet the growing demand for enhanced imaging and new therapies in fast-growing specialities such as radiotherapy, gastroenterology, inflammation, fibrosis and mitochondrial imaging.
In the USA, a rare disease is defined as one that affects no more than 200,000 individuals nationwide (a prevalence of roughly six per 10,000), and in Europe as one that affects five per 10 000, or around 250,000 individuals. Most current treatments are supportive rather than disease-modifying, leaving the majority of rare disease patients with considerable unmet medical needs.
The design and delivery of clinical trials in the rare disease arena bring specific considerations and potential pitfalls for researchers, patients, pharmaceutical companies, and regulators. Examples of trial-related questions/issues that need to be addressed include recruitment targets, dropout rates, and, ultimately, challenges of regulatory approval if the criteria for efficacy and safety are met.
As a requirement, most rare disease clinical trials are multicentre, and often multinational for sufficient patient recruitment, even in phase I and II trials. This can challenge clinical study protocol harmonization, the selection of appropriate biomarkers, ethical review, site IRB approval, indemnity, organization of clinical services, standards of care, and cultural diversity.
Watch Video
Reliable imaging services help a small biotech advance the development of a novel,rare neurological disease treatment.
Additionally, while it’s true that every patient matters in all clinical trials, this takes on new meaning in studies of rare diseases. As there are not many people living with the diagnosis, finding patients and keeping them engaged in clinical trials is critical. Trial sponsors can’t risk a patient dropping out of a study because of missteps or problems with data collection and reporting during investigator visits.
As a result, the development of new treatments for rare disease poses unique challenges to clinical trial sponsors. Because these trials can’t risk anything going wrong, sponsors need experienced partners they can rely on to get it right the first time – and every time.
Below is a collection of materials that highlight Calyx’s experience in supporting rare disease clinical trials and how our scientific and technical expertise is helping researchers successfully develop novel treatments to bring new hope to patients living with rare disease.